Yes, Advanced Brain Imaging Shows Lyme Disease Brain Fog is Real!
Lyme-disease-associated persistent symptoms include severe fatigue, pain, and cognitive problems. These symptoms can be impairing and yet difficult to validate using currently available diagnostic tests.
Patients are often told by their health practitioners: “your tests are normal, your symptoms are in your head,” aka psychosomatic.
However using advanced neuroimaging research modalities, such as PET imaging, functional MRI (fMRI), and diffusion tensor imaging (DTI), clinical researchers at Johns Hopkins University School of Medicine have identified objective inflammatory, functional, and structural abnormalities in the brains of Lyme disease patients as compared to healthy controls.
These novel findings indicate that Lyme-disease-associated cognitive symptoms are biologic and measurable, not psychosomatic.
These discoveries, although significant, are not yet well known by the physician community or presently available to clinicians.
What is brain fog?
Brain fog is a term used to describe difficulties with cognitive functions such as:
- concentrating
- word recall
- processing speed
- working memory
- mental fatigue
- multitasking
Working memory enables one to do tasks quickly or easily solve a problem without looking up information. This includes quickly learning a new computer program or using names or numbers for a routine task.
Mental fatigue is akin to how one feels after taking a long test that requires remembering detailed information or doing a complicated mental task when short on sleep.
Brain fog is difficult to diagnose
The cognitive difficulties experienced by Lyme disease patients are often too subtle for most clinical diagnostic tests to presently uncover. Standardized neuropsychological tests do reveal that working memory and processing speed are impacted, but these findings can be difficult to interpret.2 Advanced neuroimaging methodologies are more sensitive but are currently only available in a research setting.
Research utilizing advanced neuroimaging reveals novel findings
Non-standard research-grade brain neuroimaging technologies have enabled the discovery of marked biologic abnormalities in patients with Lyme disease as compared to healthy controls.
- A Columbia University brain PET imaging study (2009) found hypometabolism in Lyme-disease-associated encephalopathy.3
- A Johns Hopkins University School of Medicine brain PET imaging study (2018) revealed increased. inflammation and glial activation in patients with Lyme-disease-associated persistent symptoms.4
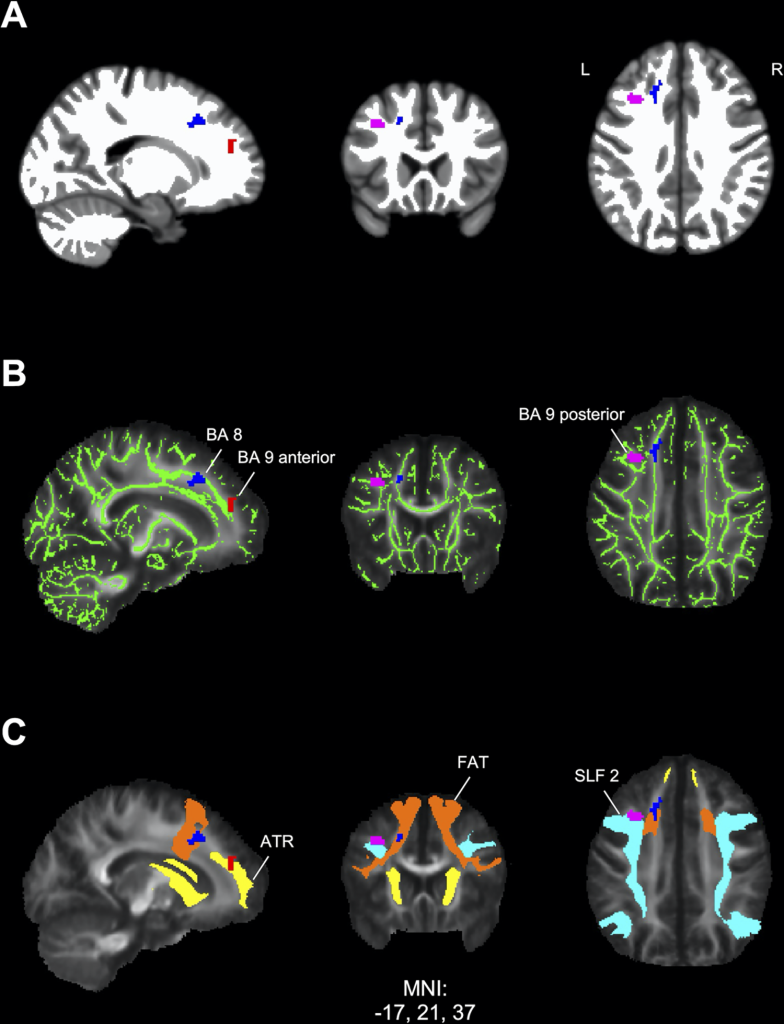
- A 2022 Johns Hopkins University School of Medicine neuroimaging study, utilizing fMRI and DTI brain scans in conjunction with each other, identified striking functional abnormalities as well as distinct structural changes in the white brain matter of Lyme disease patients.1
These findings indicate the cognitive symptoms of Lyme disease patients are real and may be associated with ongoing neuroinflammation.
More research is needed to better understand the diagnostic and therapeutic implications of these discoveries to bring new insights and advanced tools into clinical care for patients. With recent NIH support, our research is tracking brain changes in patients from the initial stages of acute Lyme disease through the first year of illness. This work uses advanced brain imaging to provide objective evidence of neurological changes and aims to identify biomarkers that could help predict and improve outcomes for patients with Lyme disease-related brain effects.
Citations:
- Marvel CL, Alm KH, Bhattacharya D, Rebman AW, Bakker A, Morgan OP, et al. (2022) A multimodal neuroimaging study of brain abnormalities and clinical correlates in post treatment Lyme disease. PLoS ONE 17(10): e0271425. https://doi.org/10.1371/journal.pone.0271425 ↩︎
- Touradji P, Aucott JN, Yang T, Rebman AW, Bechtold KT. Cognitive Decline in Post-treatment Lyme Disease Syndrome. Arch Clin Neuropsychol. 2019 Jun 1;34(4):455-465. doi: 10.1093/arclin/acy051. PMID: 29945190. https://pubmed.ncbi.nlm.nih.gov/29945190/ ↩︎
- Fallon BA, Lipkin RB, Corbera KM, Yu S, Nobler MS, Keilp JG, Petkova E, Lisanby SH, Moeller JR, Slavov I, Van Heertum R, Mensh BD, Sackeim HA. Regional cerebral blood flow and metabolic rate in persistent Lyme encephalopathy. Arch Gen Psychiatry. 2009 May;66(5):554-63. doi: 10.1001/archgenpsychiatry.2009.29. PMID: 19414715. https://pubmed.ncbi.nlm.nih.gov/19414715/ ↩︎
- Coughlin JM, Yang T, Rebman AW, Bechtold KT, Du Y, Mathews WB, Lesniak WG, Mihm EA, Frey SM, Marshall ES, Rosenthal HB, Reekie TA, Kassiou M, Dannals RF, Soloski MJ, Aucott JN, Pomper MG. Imaging glial activation in patients with post-treatment Lyme disease symptoms: a pilot study using [11C]DPA-713 PET. J Neuroinflammation. 2018 Dec 19;15(1):346. doi: 10.1186/s12974-018-1381-4. PMID: 30567544; PMCID: PMC6299943. https://pubmed.ncbi.nlm.nih.gov/30567544/ ↩︎


