Summary
A Johns Hopkins study found that males with early Lyme disease had stronger antibody responses and more severe illness than females, particularly compared with pre-menopausal females, despite having a similar duration of illness before diagnosis. Males showed higher frequencies of larger EM rashes, positive two-tier serology, elevated liver function tests, and higher neutrophil-to-lymphocyte ratios than pre-menopausal females. Post-menopausal females tended to resemble males across these objective severity markers. The findings indicate that biological sex-based differences and menopause status may influence how Lyme disease presents, progresses, and is diagnosed.
Early Lyme Disease Severity by Sex and Menopausal Status
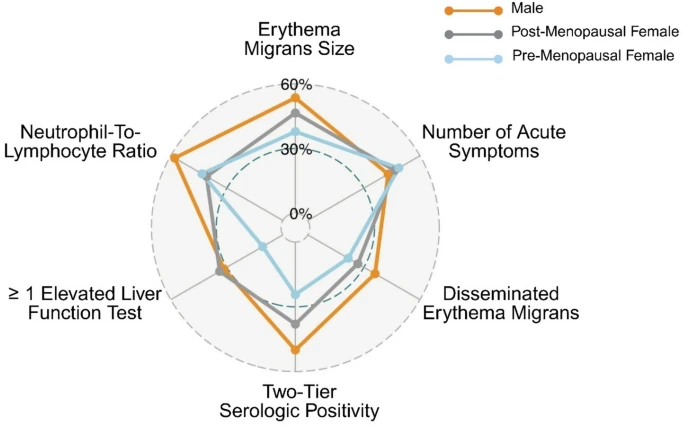
Proportion of patients with more severe early Lyme disease features, by sex and menopausal status, across objective severity markers.
Why was this study done?
Researchers set out to learn whether early Lyme disease presents differently in males and females, and whether menopause status affects these differences. Previous research has shown that sex hormones influence immune response and disease severity in many infections, but little is known about how this applies to Lyme disease. The study aimed to better understand how biological sex and hormonal status might shape the body’s immune and clinical responses to Borrelia burgdorferi infection.
How was this study done?
The research team analyzed data from 243 adults with well-characterized early Lyme disease, using data at time of diagnosis before treatment and again about three weeks later at the end of antibiotic treatment. They compared 125 males and 118 females and, among women, compared those who had gone through menopause with those who had not. The study examined reported symptoms, physical exam findings, and laboratory results, including standard two-tier antibody testing for Lyme disease.
What were the major findings?
The study found that males were more likely than females to have a positive two-tier antibody test for acute Lyme disease. Males also showed more pronounced and more severe early disease based on objective clinical markers such as larger rashes, more frequent elevations in routine laboratory measures including liver function tests and white blood cell ratios, and a higher overall disease severity score. When the researchers looked specifically at females by menopausal status, post-menopausal females resembled males more closely than pre-menopausal females in both test positivity and acute disease severity, suggesting that menopause related changes in hormones may influence immune response and clinical presentation.
Males and females reported a similar number of symptoms overall, but the types of symptoms differed. Females more often reported heart palpitations, vomiting, and sensitivity to light, while males more frequently reported sleep disruption. These differences were not due to delayed care, because males and females had similar durations of illness at the time of diagnosis.
What is the impact of this work?
This study shows that biological sex-based differences, including hormonal changes associated with menopause, may shape how the immune system responds to Lyme disease infection and may influence disease severity. Prior research has found that males are somewhat more likely to be reported with early Lyme disease and are more represented in serious untreated complications such as Lyme carditis and arthritis, while females are more likely to experience long lasting symptoms after treatment, a pattern that is similar to other post-acute infection illnesses such as long COVID, and ME/CFS.
These findings suggest that immune system activation and antibody responses may differ by biological sex and hormone levels, reflecting underlying biological and immunological influences on disease expression. Recognizing these sex-based and menopause-related differences could improve how Lyme disease is diagnosed and understood, guide future research into immune responses to infection, and help explain why younger females may be at greater risk for delayed diagnosis or persistent symptoms. This work highlights the importance of including sex and hormonal status as key biological variables in Lyme disease research and clinical assessment.
Study team members:
Alison W Rebman1*, Ting Yang1, John N Aucott1*
1Lyme Disease Research Center, Division of Rheumatology, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD USA.
This research was supported by:
This work was supported by the Steven & Alexandra Cohen Foundation, the Global Lyme Alliance, and the Bay Area Lyme Foundation.


