It is Real and Has an Identifiable Biological Basis
Several published peer-reviewed studies conducted by the Johns Hopkins Lyme Disease Research Center are generating a growing body of evidence that Lyme disease associated persistent symptoms are biologically driven and not psychosomatic.
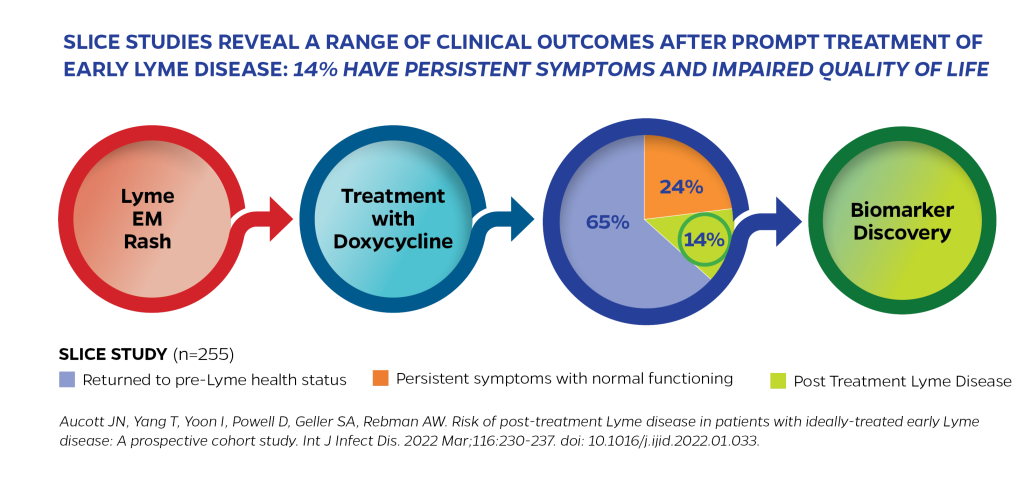
One study, led by Center Director, John Aucott, MD, found that 14% of patients who received early, standard antibiotic treatment for acute Lyme disease still developed persistent, functionally impairing symptoms, known as post-treatment Lyme disease (PTLD). This research confirms that Lyme disease can cause significant, long-lasting symptoms, such as severe fatigue, body pain and cognitive difficulties, even when treatment is started promptly. These lingering symptoms can substantially reduce quality of life and are not explained by everyday fatigue or pain. Although new cases of depression and anxiety may develop after chronic Lyme disease has been established, the Center’s research indicates that these symptoms are often consequences of the chronic illness rather than its initial cause.
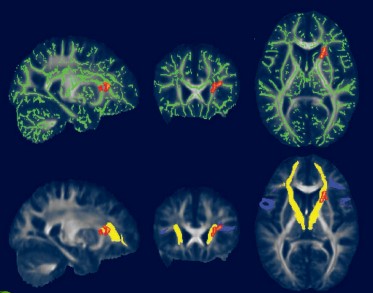
Cherie Marvel, PhD, Associate Professor of Neurology at Johns Hopkins, leads research using advanced MRI brain imaging techniques that objectively demonstrate structural and functional brain changes in Lyme disease patients, providing clear scientific evidence that Lyme disease-associated brain fog is real and a biologically based condition. Dr. Marvel’s novel research reveals significant insights into unexpected white matter changes in patients with chronic symptoms and post-treatment Lyme disease (PTLD).
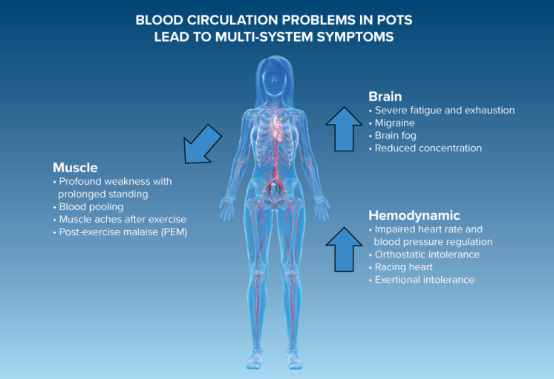
Brit Adler, MD, Assistant Professor of Medicine, works with Lyme disease patients suffering with dysautonomia and POTS to identify autonomic nervous system dysfunction that previously was unrecognized and that may also contribute to cognitive problems and symptoms of anxiety and depression.
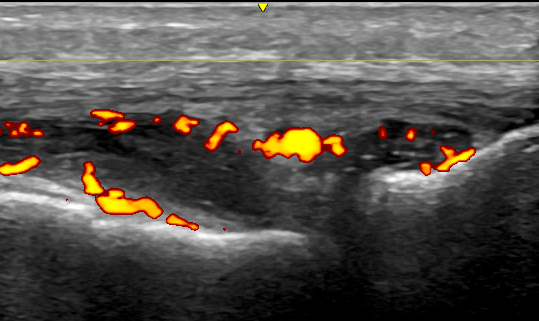
John Miller, MD, Assistant Professor of Medicine at Johns Hopkins, has published evidence that some people with persistent pain after acute Lyme disease can have ongoing joint inflammation, which may frequently be subtle and unrecognized, but can be detected by musculoskeletal ultrasound.
Our research also shows Lyme disease patients exhibit different microbiome, metabolome, gene regulation and epigenetic patterns, and immune responses compared to healthy controls.
Meaningful scientific progress begins with LISTENING TO OUR PATIENTS.
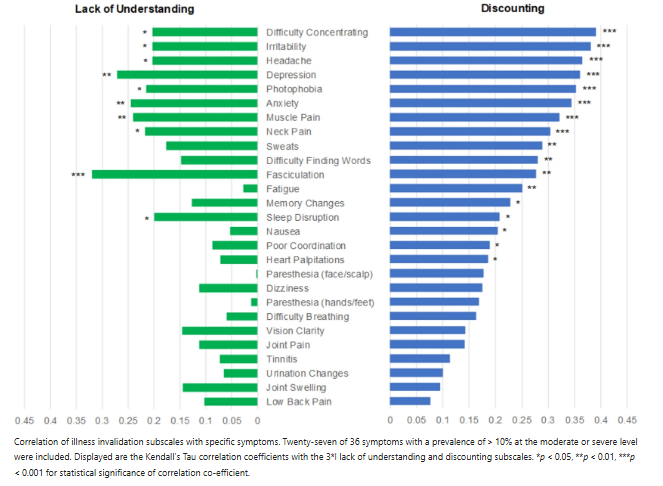
Qualitative research by Alison Rebman, MPH, Assistant Professor, Johns Hopkins University School of Medicine and the Lyme Disease Research Center’s Director for Clinical and Epidemiological Research, has documented the significance of the patient’s illness narrative and underscored how crucial healthcare provider validation of a patient’s story can be. By actively engaging with our patients’ experiences and concerns, we ensure that our research remains grounded in real-world needs and perspectives. Alison’s qualitative research complements the objective biological evidence that demonstrates Lyme disease is not a psychosomatic illness.
In our clinic, our multidisciplinary team continues to uncover features of the patient’s illness that demonstrate Lyme disease is being driven by complex biological processes such as inflammation, dysautonomia and dysregulated immune responses and is not a psychosomatic illness.
Our goal is to translate research findings into more accurate diagnostics and effective treatments, ultimately improving the lives of those affected by Lyme disease.


